Prostatitisis an inflammatory disease of the prostate. Manifested by frequent urination, pain in the penis, scrotum, rectum, sexual disorders (erection dysfunction, premature ejaculation, etc. ), sometimes urinary retention, blood in the urine. The diagnosis of prostatitis is established by a urologist or an andrologist according to a typical clinical picture, the results of a digital rectal examination. Additionally, ultrasound of the prostate, bakposev of prostatic secretion and urine is performed. Treatment is conservative - antibiotic therapy, immunotherapy, prostate massage, lifestyle correction.
general informations
Prostatitis is an inflammation of the seminal gland (prostate) - the prostate. It is the most common disease of the genitourinary system in men. Most often affects patients aged 25-50 years. According to various data, 30-85% of men over 30 suffer from prostatitis. Possible formation of prostate abscess, inflammation of the testicles and appendages, which threatens infertility. The rise of the infection leads to inflammation of the upper genitourinary system (cystitis, pyelonephritis).
Pathology develops with the penetration of an infectious agent that enters the prostate tissue from the organs of the genitourinary system (urethra, bladder) or from a distant inflammatory focus (with pneumonia, influenza, tonsillitis, furunculosis).
Prostate adenoma is a benign tumor of the paraurethral glands located around the urethra in its prostatic section. The main symptom of prostate adenoma is a violation of urination due to the gradual compression of the urethra by one or more growing nodules. The pathology is characterized by a benign course.
Only a small part of patients consult a doctor, however, a detailed examination reveals the symptoms of the disease in one out of four men aged 40-50, and in half of men aged 50-60. The disease is detected in 65% of men aged 60-70, 80% of men aged 70-80 and more than 90% of men over 80. The severity of symptoms can vary greatly. Studies in the field of clinical andrology suggest that problems with urination occur in approximately 40% of men with BPH, but only one in five patients in this group consult a doctor.
Causes of prostatitis
As an infectious agent in an acute process, Staphylococcus aureus (Staphylococcus aureus), Enterococcus (Enterococcus), Enterobacter (Enterobacter), Pseudomonas (Pseudomonas), Proteus (Proteus), Klebsiella (Klebsiella) and Escherichia coli (E. Coli)can act. Most microorganisms belong to the conditionally pathogenic flora and cause prostatitis only in the presence of other predisposing factors. Chronic inflammation is usually due to polymicrobial associations.
The risk of developing the disease increases with hypothermia, a history of specific infections, and conditions accompanied by congestion in the tissues of the prostate. There are the following predisposing factors:
- General hypothermia (punctual or permanent, related to working conditions).
- A sedentary lifestyle, a specialty that requires a person to sit for a long time (computer scientist, driver, etc. ).
- Constant constipation.
- Violations of the normal rhythm of sexual activity (excessive sexual activity, prolonged abstinence, incomplete ejaculation during "usual" sexual intercourse devoid of emotional coloring).
- The presence of chronic diseases (cholecystitis, bronchitis) or chronic infectious foci in the body (chronic osteomyelitis, untreated caries, tonsillitis, etc. ).
- Past urological diseases (urethritis, cystitis, etc. ) and sexually transmitted diseases (chlamydia, trichomoniasis, gonorrhea).
- Conditions that cause immune system suppression (chronic, irregular stress and malnutrition, lack of regular sleep, overtraining in athletes).
It is assumed that the risk of developing pathology increases with chronic intoxication (alcohol, nicotine, morphine). Some studies in the field of modern andrology prove that chronic perineal trauma (vibration, concussion) in motorists, bikers and cyclists is a provoking factor. However, the vast majority of experts believe that all these circumstances are not the real causes of the disease, but only contribute to the exacerbation of the latent inflammatory process in the tissues of the prostate.
A decisive role in the onset of prostatitis is played by congestion of prostate tissue. Violation of capillary blood flow causes increased lipid peroxidation, edema, exudation of prostate tissues and creates conditions for the development of an infectious process.
The mechanism of development of prostate adenoma has not yet been fully determined. Despite the widespread opinion linking the pathology with chronic prostatitis, there are no data that would confirm the link between these two diseases. Researchers found no relationship between the development of prostate adenoma and alcohol and tobacco consumption, sexual orientation, sexual activity, sexually transmitted and inflammatory diseases.
There is a pronounced dependence of the incidence of prostate adenoma on the age of the patient. Scientists believe that adenoma develops as a result of hormonal imbalances in men during andropause (male menopause). This theory is supported by the fact that men castrated before puberty never suffer from pathology, and extremely rarely - men castrated after.
Symptoms of prostatitis
Acute prostatitis
There are three stages of acute prostatitis, which are characterized by the presence of a certain clinical picture and morphological changes:
- Acute catarrhal. Patients complain of frequent and often painful urination, pain in the sacrum and perineum.
- Acute follicular. The pain becomes more intense, sometimes radiating to the anus, aggravated by defecation. Urination is difficult, urine flows in a thin stream. In some cases, there is urinary retention. A subfebrile state or moderate hyperthermia is typical.
- Acute parenchymal. Severe general intoxication, hyperthermia up to 38-40°C, chills. Dysuric disorders, often - acute urinary retention. Sharp and shooting pains in the perineum. Difficulty defecating.
Chronic prostatitis
In rare cases, chronic prostatitis becomes the result of an acute process, however, as a rule, a primary chronic course is observed. The temperature sometimes rises to subfebrile values. The patient notes a slight pain in the perineum, discomfort during the act of urination and defecation. The most characteristic symptom is scanty discharge from the urethra during defecation. The primary chronic form of the disease develops over a considerable period of time. It is preceded by prostatosis (blood stagnation in the capillaries), gradually transforming into abacterial prostatitis.
Chronic prostatitis is often a complication of the inflammatory process caused by the causative agent of a specific infection (chlamydia, trichomonas, ureaplasma, gonococcus). Symptoms of a specific inflammatory process in many cases mask the manifestations of prostate damage. Perhaps a slight increase in pain during urination, slight pain in the perineum, little discharge from the urethra during defecation. A slight change in the clinical picture often goes unnoticed by the patient.
Chronic inflammation of the prostate can be manifested by a burning sensation in the urethra and perineum, dysuria, sexual disorders, increased general fatigue. The consequence of violations of potency (or fear of these violations) often becomes mental depression, anxiety and irritability. The clinical picture does not always include all listed symptom groups, differs between patients and changes over time. There are three main characteristic syndromes of chronic prostatitis: pain, dysuria, sexual disorders.
There are no pain receptors in prostate tissue. The cause of pain in chronic prostatitis becomes almost inevitable due to the abundant innervation of the pelvic organs, involvement in the inflammatory process of the nerve pathways. Patients complain of pain of varying intensity - from weak and painful sleep to intense and disturbing sleep. There is a change in the nature of the pain (intensification or weakening) with ejaculation, excessive sexual activity or sexual abstinence. The pain radiates to the scrotum, sacrum, perineum, sometimes to the lumbar region.
As a result of inflammation in chronic prostatitis, the volume of the prostate increases, compressing the urethra. The lumen of the ureter is reduced. The patient has frequent urges to urinate, a feeling of incomplete emptying of the bladder. As a rule, dysuric phenomena are expressed in the early stages. Then, a compensatory hypertrophy of the muscle layer of the bladder and ureters develops. Symptoms of dysuria during this period weaken, then increase again with the decompensation of adaptive mechanisms.
In the early stages, dyspotence may develop, which manifests differently in different patients. Patients may complain of frequent nocturnal erections, blurry orgasm, or worsening erections. Accelerated ejaculation is associated with a decrease in the orgasmic center arousal threshold. Painful sensations during ejaculation can cause refusal of sexual activity. In the future, sexual dysfunctions become more pronounced. In the advanced stage, impotence develops.
The degree of sexual disorder is determined by many factors, including the patient's sexual constitution and psychological mood. Violations of potency and dysuria can be due both to changes in the prostate gland and to the suggestibility of the patient, who, if he has chronic prostatitis, expects the inevitable development of sexual disorders and disorders ofurination. Especially often, psychogenic dyspotence and dysuria develop in suggestible and anxious patients.
Impotence, and sometimes even the threat of possible sexual disorders, is difficult for patients to tolerate. Often there is a change of character, irritability, obnoxiousness, excessive concern for one's own health, and even "care of illness. "
There are two groups of disease symptoms: irritative and obstructive. The first group of symptoms includes increased urination, persistent (imperative) urge to urinate, nocturia, urinary incontinence. The group of obstructive symptoms includes difficulty urinating, delayed onset and increased time of urination, a feeling of incomplete emptying, urination with an intermittent slow stream, the need to strain. There are three stages of prostate adenoma: compensated, undercompensated, and decompensated.
Compensated step
At the compensated stage, the dynamics of the act of urination change. It becomes more frequent, less intense and less free. It is necessary to urinate 1-2 times at night. Typically, nocturia in stage I prostate adenoma is not of concern in a patient who associates constant nocturnal awakenings with the development of age-related insomnia. During the day, the normal frequency of urination can be maintained, however, patients with stage I prostate adenoma note a waiting period, especially pronounced after a night's sleep.
Then the frequency of daytime urination increases and the volume of urine released per urination decreases. There are imperative desires. The flow of urine, which previously formed a parabolic curve, is discharged slowly and falls almost vertically. Hypertrophy of the muscles of the bladder develops, due to which the efficiency of its emptying is maintained. There is little or no residual urine in the bladder at this stage (less than 50ml). The functional state of the kidneys and upper urinary tract is preserved.
Undercompensated stage
In stage II of prostate adenoma, the bladder increases in volume, dystrophic changes develop in its walls. The amount of residual urine is more than 50 ml and continues to increase. Throughout the act of urinating, the patient is forced to intensely strain the abdominal muscles and the diaphragm, which leads to an even greater increase in intravesical pressure.
The act of urinating becomes multiphasic, intermittent, undulating. The passage of urine along the upper urinary tract is gradually disturbed. Muscle structures lose their elasticity, the urinary tract expands. Renal function is impaired. Patients worry about thirst, polyuria, and other symptoms of progressive chronic kidney failure. When the compensation mechanisms fail, the third stage begins.
Decompensated stage
The bladder in patients with stage III prostate adenoma is stretched, filled with urine, easily determined by palpation and visually. The upper edge of the bladder can reach the level of the navel and above. Emptying is impossible even with intense tension of the abdominal muscles. The desire to empty the bladder becomes continuous. There may be severe pain in the lower abdomen. Urine is excreted frequently, in drops or in very small portions. In the future, the pain and the urge to urinate gradually weaken.
A characteristic paradoxical urinary retention develops, or paradoxical ischuria (the bladder is full, urine is constantly excreted drop by drop). The upper urinary tract is enlarged, the functions of the renal parenchyma are impaired due to the constant obstruction of the urinary tract, leading to increased pressure in the pelvicalyceal system. The clinic of chronic renal failure develops. If medical care is not provided, patients die from progressive CKD.
Complications
In the absence of timely treatment of acute prostatitis, there is a significant risk of developing a prostate abscess. With the formation of a purulent focus, the patient's body temperature rises to 39-40 ° C and can become hectic in nature. Periods of heat alternate with violent chills. Sharp pains in the perineum make urination difficult and defecation impossible.
Increased prostatic edema leads to acute retention of urine. Rarely, an abscess ruptures spontaneously in the urethra or rectum. When opened, purulent, cloudy urine with an unpleasant pungent odor appears in the urethra; when opened, the feces contain pus and mucus in the rectum.
Chronic prostatitis is characterized by an undulating course with periods of long-term remissions, during which the inflammation of the prostate is latent or manifests itself with extremely weak symptoms. Patients who are not bothered by anything often stop treatment and only turn around when complications develop.
The spread of infection through the urinary tract provokes the appearance of pyelonephritis and cystitis. The most common complication of the chronic process is inflammation of the testicles and epididymis (epdidymo-orchitis) and inflammation of the seminal vesicles (vesiculitis). The result of these diseases is often infertility.
Diagnostic
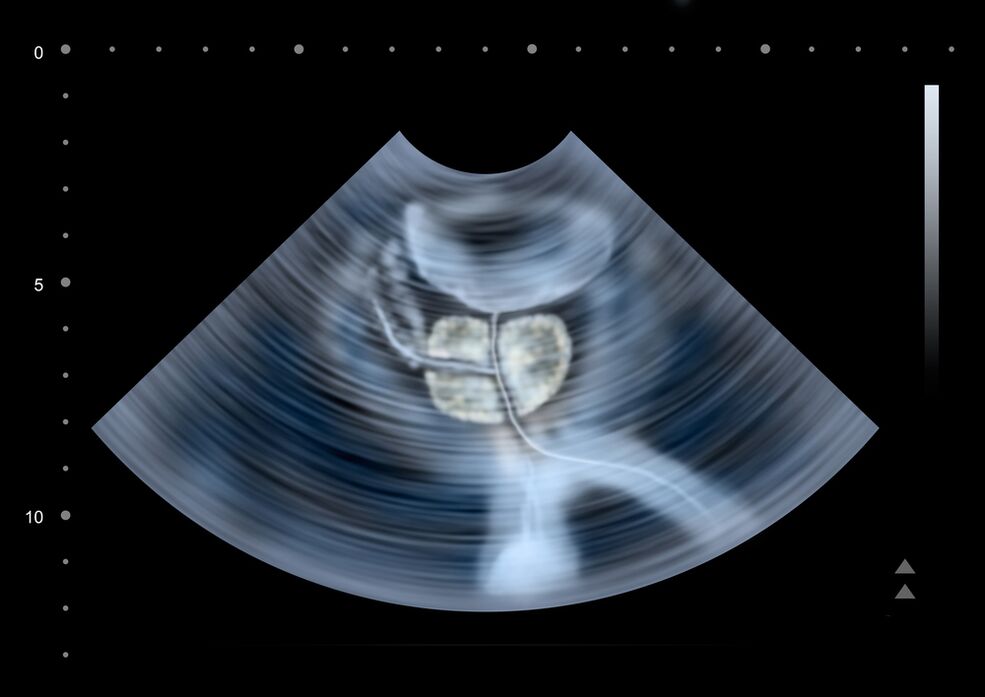
In order to assess the severity of symptoms of prostate adenoma, the patient is asked to complete a voiding diary. During the consultation, the urologist performs a digital examination of the prostate. To exclude infectious complications, a swab and examination of the secretion of the prostate and smears from the urethra are performed. Additional tests include:
- Ultrasound.During prostate ultrasound, the volume of the prostate is determined, stones and congested areas are detected, the amount of residual urine, the condition of the kidneys and urinary tract are assessed.
- Urodynamic study. Uroflowmetry allows you to reliably judge the degree of urinary retention (the timing of urination and the speed of urine flow are determined by a special device).
- Definition of tumor markers.To exclude prostate cancer, the level of PSA (prostate specific antigen) must be evaluated, the value of which should normally not exceed 4 ng/ml. In controversial cases, a prostate biopsy is performed.
Cystography and excretory urography of prostate adenoma have been performed less frequently in recent years due to the emergence of new, less invasive and safer research methods (ultrasound). Sometimes a cystoscopy is done to rule out diseases with similar symptoms or in preparation for surgical treatment.
Treatment of prostatitis
Treatment of acute prostatitis
Patients with an uncomplicated acute process are treated by an outpatient urologist. In case of severe poisoning, suspicion of a purulent process, hospitalization is indicated. Antibacterial treatment is carried out. Preparations are selected taking into account the susceptibility of the infectious agent. Antibiotics are widely used and can penetrate prostate tissue well.
With the development of acute urinary retention on the end of prostatitis, they resort to the installation of a cystostomy, and not a urethral catheter, since there is a risk of the formation of a prostate abscess. With the development of an abscess, a transrectal or transurethral endoscopic opening of the abscess is performed.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should be complex, including etiotropic therapy, physiotherapy, correction of immunity:
- Antibiotic therapy. The patient is prescribed long courses of antibacterial drugs (within 4-8 weeks). The selection of the type and dosage of antibacterial drugs, as well as the determination of the duration of treatment are carried out individually. The drug is selected based on the sensitivity of the microflora based on the results of urine culture and prostate secretion.
- Prostate massage.Massage of the gland has a complex effect on the affected organ. During the massage, the inflammatory secret accumulated in the prostate is expelled through the ducts, then enters the urethra and is evacuated from the body. The procedure improves blood circulation in the prostate, which minimizes congestion and ensures better penetration of antibacterial drugs into the tissues of the affected organ.
- Physiotherapy.To improve blood circulation, laser exposure, ultrasonic waves and electromagnetic vibrations are used. If it is impossible to perform physiotherapeutic procedures, the patient is prescribed warm medicinal microclysters.
In long-term chronic inflammation, consultation with an immunologist is indicated to select immunocorrective treatment tactics. The patient receives advice on lifestyle changes. Making certain changes in the lifestyle of a patient with chronic prostatitis is both curative and preventive. The patient is recommended to normalize sleep and wakefulness, establish a diet, conduct moderate physical activity.
Conservative therapy
Conservative therapy is carried out in the early stages and in the presence of absolute contraindications to surgery. To reduce the severity of the symptoms of the disease, alpha-blockers, 5-alpha reductase inhibitors, herbal preparations (extract from the bark of African plum or sabal fruit) are used.
Antibiotics are prescribed to fight the infection that often accompanies prostate adenoma. At the end of antibiotic treatment, probiotics are used to restore normal intestinal microflora. Perform immunity correction. The atherosclerotic vascular changes that develop in most elderly patients impede the flow of drugs into the prostate gland. So special drugs are prescribed to normalize blood circulation.
Operation
There are the following surgical methods for the treatment of prostate adenoma:
- ROUND(transurethral resection). Minimally invasive endoscopic technique. The operation is performed with an adenoma volume of less than 80 cm3. Not applicable in case of renal insufficiency.
- Adenomectomy.It is performed in the presence of complications, the mass of the adenoma is greater than 80 cm3. Currently, laparoscopic adenomectomy is widely used.
- Laser vaporization of the prostate.Allows to perform surgery with a tumor mass of less than 30-40 cm3. It is the method of choice for young patients with prostate adenoma, because it helps to safeguard sexual function.
- Laser enucleation(holmium - HoLEP, thulium - ThuLEP). The method is recognized as the "gold standard" for surgical treatment of prostate adenoma. Allows the removal of an adenoma with a volume greater than 80 cm3 without open surgery.
There are a number of absolute contraindications to the surgical treatment of prostate adenoma (decompensated diseases of the respiratory and cardiovascular systems, etc. ). If surgical treatment is not possible, bladder catheterization or palliative surgery is performed - cystostomy, placement of a urethral stent.
Forecast and prevention
Acute prostatitis is a disease that has a strong tendency to become chronic. Even with timely and adequate treatment, more than half of patients end up with chronic prostatitis. Recovery is far from always achieved, however, with the correct and consistent treatment and following the doctor's recommendations, it is possible to eliminate unpleasant symptoms and achieve long-term stable remission in a chronic process.
Prevention consists of eliminating risk factors. It is necessary to avoid hypothermia, to alternate sedentary work and periods of physical activity, to eat regularly and fully. For constipation, laxatives should be used. One of the preventive measures is the normalization of sexual life, since excessive sexual activity and sexual abstinence are risk factors in the development of prostatitis. If symptoms of a urological or sexually transmitted disease appear, you should consult a doctor in a timely manner.























